Also, make sure to use a HIPPS code.
![]()
From: Marnie Pogreba
Sent: Thursday, February 10, 2022 3:23 PM
To: billers@list.mnhomecare.org
Subject: RE: Payor MEDM1
You will want to follow Medicare PDGM rules.
Bill the final claim with Type of Bill: 329.
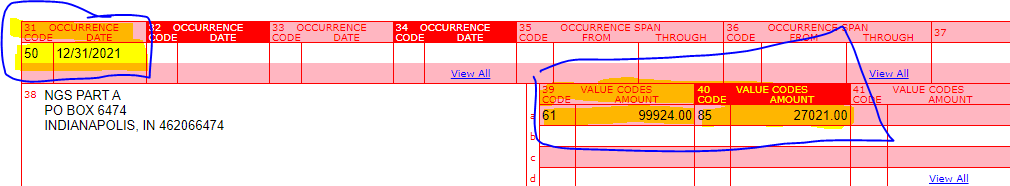
Make sure these codes (see example below) are entered with the appropriate date for Occurrence Code 50 and the Value Codes for your agency. You could look at one of your Medicare claims to get an idea. The Value Code 85 and the amount
is specific to where the patient lives.
From: billers@list.mnhomecare.org <billers@list.mnhomecare.org>
On Behalf Of Sara Sundberg
Sent: Wednesday, February 09, 2022 4:40 PM
To: billers@list.mnhomecare.org
Subject: Re: Payor MEDM1
|
**External Sender** |
Hello,
I am fairly new to the list, so I may have missed this conversation. I am getting denials on this payer for "invalid present on admission indicator for type of bill." What indicators have you all been using to get paid?
Thank you!
Sara
On Tue, Dec 21, 2021 at 2:41 PM Patti Fladwood <pfladwood@preshomes.org> wrote:
We send the 61 and 85 value codes, the occurrence 50 code, the hipps code and the q codes and the type of bill has to be 329. Since we’ve added all those elements we have been getting paid.
From: billers@list.mnhomecare.org <billers@list.mnhomecare.org> On Behalf Of Mary Hanson
Sent: Tuesday, December 21, 2021 1:42 PM
To: billers@list.mnhomecare.org
Subject: RE: Payor MEDM1
Anyone have any luck getting these claims to pay by including the HIPPS code on the claims?
From: billers@list.mnhomecare.org <billers@list.mnhomecare.org>
Sent: Wednesday, October 27, 2021 4:16 PM
To: billers@list.mnhomecare.org
Subject: RE: Payor MEDM1
We are having the same issue. We are now sending corrected claims to include the HIPPS code on claims, as this seems to be the reason for the take backs. We have not yet had any claims reprocess, however, so I’m not 100% sure this will be what they are looking for.
From: billers@list.mnhomecare.org <billers@list.mnhomecare.org> On Behalf Of Mary Hanson
Sent: Wednesday, October 27, 2021 4:05 PM
To: billers@list.mnhomecare.org
Subject: Payor MEDM1
Hello!
I know a couple of weeks ago there were some emails about this Medica payor. We still have some that go back to January that they’ve denied but I have pretty much given up trying to get these to pay. Every time I talked to someone I was given a different answer on what they were looking for. We used occurrence code 50 and Rev Code 0023 as previously stated by others.
Well, they have now started taking back claims that we were paid for. The Reason is CO16 Claim/service lacks information or has submission/billing errors which is needed for adjudication and N463 which states missing support data for claim.
Has anyone gotten any where on getting these paid? Or been able to have the take back reconsidered?
Any help is greatly appreciated.
Thanks!
Mary Hanson | Billing Specialist | River Valley Home Care Inc.
916 8th Street Farmington, MN 55024
Phone: 651-460-4201
Email: mhanson@rvhci.com
CONFIDENTIALITY NOTICE: This message (including any attachments) may contain confidential client information. The information is intended only for the use of the individual or entity to whom it is addressed. If you're not the addressee or the employee or agent responsible to deliver this e-mail to its intended recipient, you are hereby notified that any review, use, dissemination, distribution, disclosure, copying or taking of any action in reliance on the contents of this information is strictly prohibited. If you have received this communication in error, please notify the sender immediately, delete this message from your computer and ask your network administrator to delete it from any storage or back up files.This electronic securemail transmission (including any attachments) may contain confidential health or other information that is protected by law. It is not intended for transmission to, or receipt by, any unauthorized persons. If you have received this electronic mail transmission in error, please delete it, and notify the sender by reply electronic mail transmission so that our records can be corrected.
--